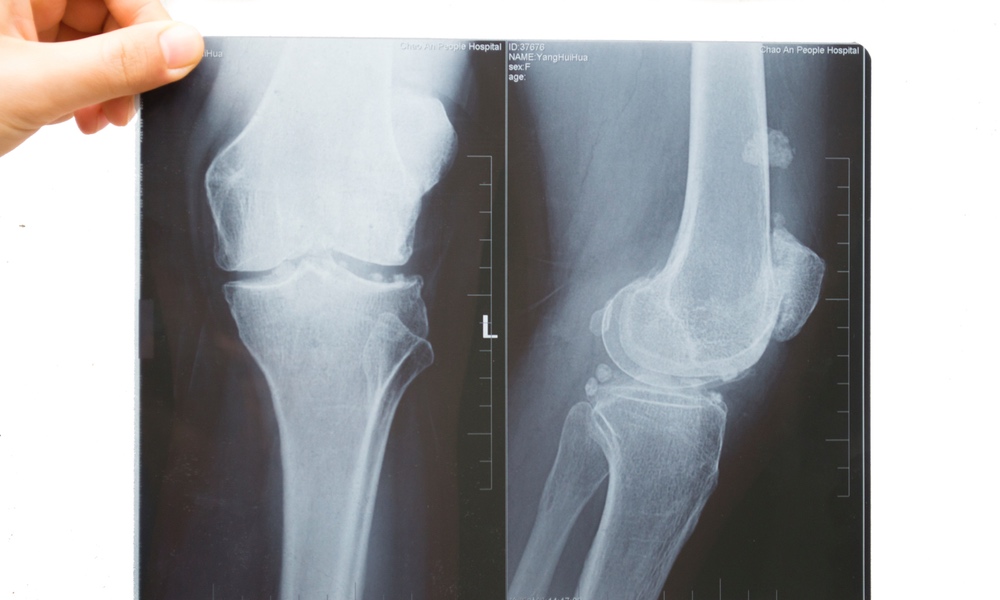
Osteoarthritis (OA) is a degenerative disease that leads to pain, stiffness, swelling of joints and is a leading cause of disability around the world. Genetics, overweight, age, injury, overuse of joints, as well as certain underlying diseases and medical conditions, can all cause the cartilage between the bones of the joints to break down. Without this shock-absorbing cartilage cushion, the bones grate against each other causing the swelling and other symptoms of osteoarthritis.
There is no specific treatment or cure for OA, but exercise, medications and surgery are all used to manage its painful symtoms. One of the major goals of research into OA is the prevention of joint and cartilage changes and trying to find ways to slow down the progression of disease and disability in those who already show symptoms.
Researchers at the University of Surrey reviewed the last ten years of osteoarthritis literature to try to come up with recommendations for measures that individuals could take to help prevent or slow down the disease.Losing weight is helpful for two reasons: It can decrease the physical load on joints, and it reduces the presence of inflammatory compounds within the joints.
Obesity is associated with a generalized low-grade inflammation with higher levels of inflammatory compounds circulating throughout the body. Their presence changes the metabolic balance within the joints and can lead to OA, making weight management potentially effective for two reasons. First, losing weight can decrease the physical load on joints. And second, weight loss reduces the presence of inflammatory compounds within the joints.
Based on the studies they reviewed, the researchers recommend that people with OA who are overweight should aim for a 10 percent weight loss and a BMI (body mass index) within the normal range. People with OA who cut back on calories need to be sure they are not compromising the intake of essential nutrients and vitamins, the researchers warn, and recommend that dieting be done in conjunction with exercise, strengthening and mobility programs that are tailored to the capabilities of the individual.
Vitamin D plays a primary role in bone health, and when it is too low, bone may not be able to protect itself from osteoarthritis. Some studies have shown an association between low vitamin D and the loss of cartilage and progression of OA, but studies on vitamin D supplements to prevent or slow OA have not been uniformly positive. Vitamin D deficiency has not been clearly shown to cause OA, but, the researchers note, when vitamin D levels are adequate, muscles are stronger and would more effectively surround and support the joint, a good reason for OA patients to make sure their vitamin D levels are adequate. Dietary sources of vitamin D include eggs, fatty fish, fortified food and beef liver.
So what can you do? There is enough evidence to make several recommendations to help prevent and delay the progression of osteoarthritis, even if the precise causes are not yet clear. It's important to take an active approach toward maintaining your joint and bone health. The recommended steps are essentially risk-free strategies that are good for general metabolic health and well-being, and which can also reduce your risk of osteoarthritis: Lose weight if you need to; get more exercise; lower your lipid intake and dietary cholesterol; eat foods that will supply the micronutrients and vitamin D that will help prevent inflammation and joint damage.
The study is published in Rheumatology.