Here's some good news: Cancer deaths continue to fall. Cancer is still the second leading cause of death in the United States, but the death rate from cancer has dropped by 27 percent since 1991. The decline seems to be the result of more people quitting smoking, as well as advances in early detection and treatment, the American Cancer Society (ACS) says.
The American Cancer Society report focuses mainly on cancer mortality rates — a measure of how many people die from a particular type of cancer in a given year.
Researchers focus on cancer mortality rates because they are relatively unaffected by all the tiny cancers we can detect today that aren't life threatening.Not all the numbers are rosy. Socioeconomic disparities remain and are rising. Poverty is associated with less cancer screening, later diagnosis and a lower likelihood of optimal treatment.
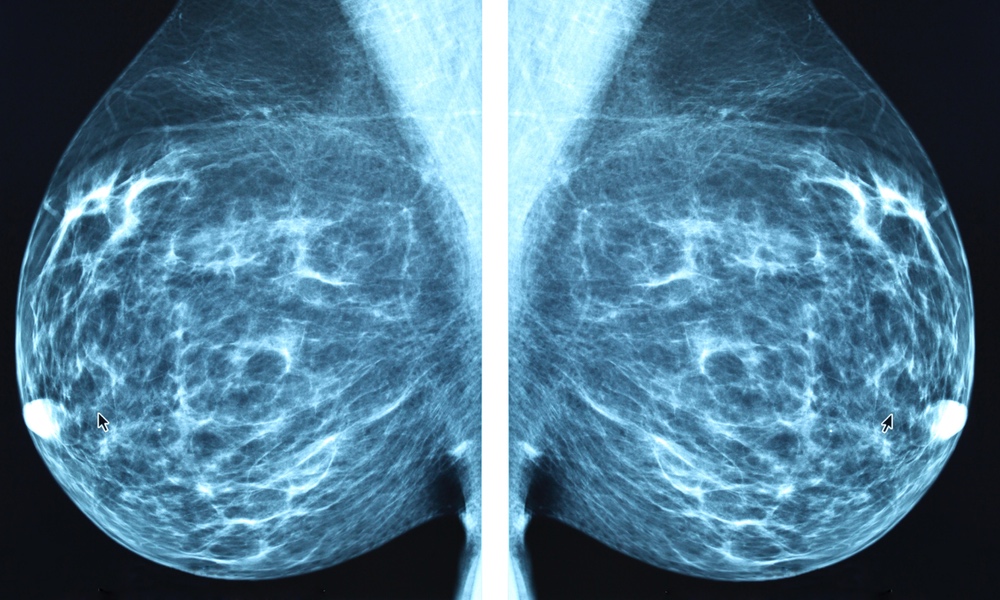
The decrease is obvious in certain cancers. The lung cancer death rate dropped by 48 percent from 1990 to 2016 among men and by two percent from 2002 to 2016 among women, with these declines accelerating in recent years. The death rate for breast cancer among women dropped by 40 percent from 1989 to 2016.
Not all cancers have seen a drop in death rates. Pancreatic cancer hasn't; it is usually diagnosed at a late stage, when treatment is largely ineffective.
In addition to a general decrease in cancer deaths, the racial disparity in cancer deaths has narrowed: In 1993, the cancer death rate of blacks was a third higher than that of whites; in 2016, it was only 14% higher. The report also attributes this progress largely to the steep drop in smoking among black teens.
Not all the numbers are rosy. Socioeconomic disparities remain and are rising. Poor people are increasingly more likely to die from cancer, a complete reversal of the pattern before 1980, when cancer mortality was lower among the poor. The most striking example of this is colorectal cancer. Mortality rates in the poorest counties for men with colorectal cancer were about 20 percent lower than those in affluent counties in the early 1970s. Now they are 35 percent higher.
Rates of smoking and obesity in the poorest counties are double those found in the wealthiest counties. Poverty is also associated with less cancer screening, later diagnosis and a lower likelihood of optimal treatment.
The report appears in CA: A Cancer Journal for Clinicians. A consumer version of the report, Cancer Facts & Figures 2019, can be found on the ACS website.