More kids than ever are hurting themselves on purpose. This type of self-harm is also known as self-injury, self-mutilation or self-abuse. No matter what it’s called, figuring out who is at the highest risk for harming themselves has been a challenge for medical providers and caregivers. But a recently-released study offers a new approach using risk profiles that can help to pinpoint which children and teens are in the most danger for hurting themselves.
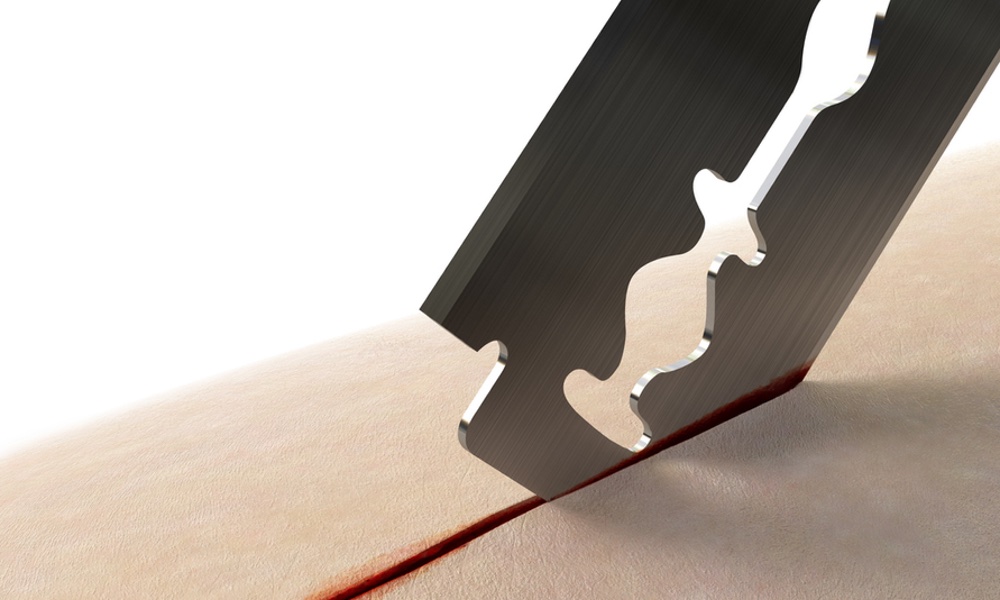
“Self-harm is a big bucket of events from mild things like cutting on the arms or thighs to taking so much Tylenol that you die on purpose or jumping out of a window, and we wanted to find out which kids require hospitalization and more intensive treatment and monitoring,” one of the study’s authors, James Antoon, said in a press release.
Records on nearly 1,100 children between the ages of 5 to 18 years who were hospitalized with a neuropsychiatric event at Monroe Carell Jr. Children’s Hospital at Vanderbilt University and the Children’s Hospital of Colorado, in Aurora, Colorado between April 2016 and March 2020 were used for the study. Of those young people, 406 (37 percent) were diagnosed with a self-harm event.Kids who self-harm often deny it and hide the evidence.
- Very high-risk consisted of boys ages 10 to 13 with ADHD, bipolar disorder, autism spectrum disorder and other developmental disorders.
- High-risk included females 14 to 17 with depression and anxiety in conjunction with substance and trauma-related disorders. Personality and eating disorders were also significant for this profile.
- Moderate risk had a significant absence of depressive disorders, suggesting that these disorders play a major role in driving the risk of suicidality.
- Low-risk consisted of children ages 5-9 who had non-mental health diagnoses such as mood disorders, behavioral disorder, psychotic disorders, developmental disorders and trauma or substance-related disorders.
“Our study provides a novel approach that takes the child’s entire medical and psychiatric profile into account and assesses what overall constellations of factors are associated with imminent self-harm,” said Antoon, an assistant professor of pediatrics and hospital medicine at Monroe Carell Jr. Children’s Hospital at Vanderbilt University in Nashville.
The team agrees further study is necessary in order to validate these risk profiles in larger populations. Real-time risk assessments for providers also need to be developed.“Self-harm is a big bucket of events from mild things like cutting on the arms or thighs to taking so much Tylenol that you die on purpose or jumping out of a window…”
- Address the issue directly. Ask your kid if their self-harming. Listen more than speaking and take a non-judgmental position. Be sure to express your love and concern. You can respond by saying something like: "This is hard for me to even think about because I care about you and want you to be healthy and safe, always."
- Be prepared to be stonewalled. Kids who self-harm often deny it and hide the evidence. Your child might get upset or refuse to talk about it. When things calm down, let your child know that you’re worried and plan to speak with their doctor about it. Make the appointment and tell your child you hope they’ll join you. If they refuse, let them know that you plan on keeping the appointment anyway.
- Trust your pediatrician. If your child agrees to go, encourage private one-on-one time for your kid with their doctor. Your pediatrician can also work with you to create a care plan geared to your child’s situation. It might include therapy, stress reduction techniques and/or medication.
- Keep your environment safe. You can help by removing hazards such as sharp knives, razors, poisons, weapons and more from your space. It is also important to keep firearms inaccessible and all medications locked away, especially if your child is having suicidal thoughts. You’ll also want to speak with your pediatrician about a safety plan, including what you should do if there’s an emergency.
The study can be found in Pediatrics.