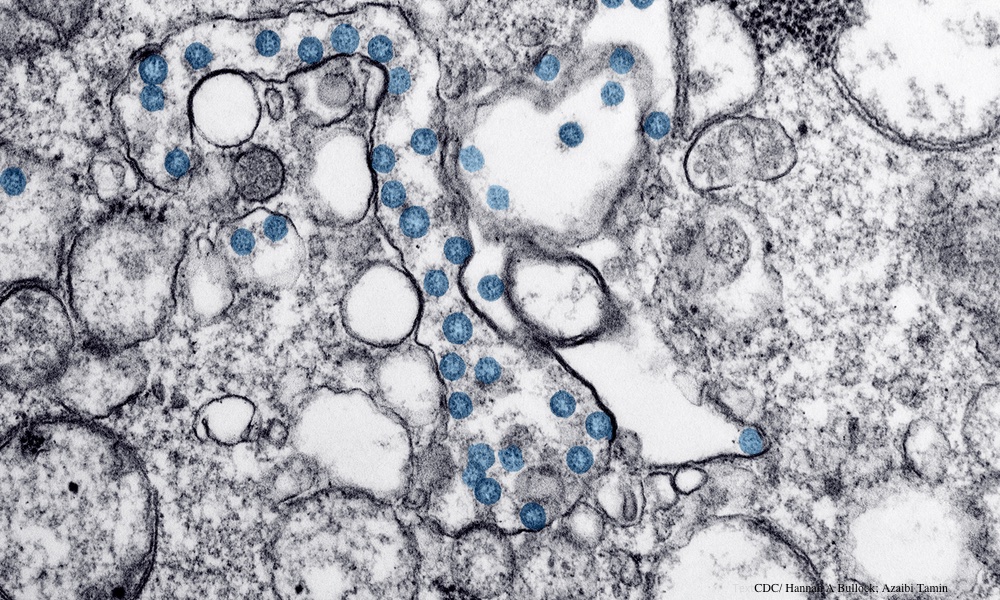
Infection with SARS-CoV-2, the virus that causes COVID-19, often includes long-term complications known as long COVID. Doctors have some understanding of the initial immune system response in patients who have severe COVID-19. The long-term effects of the virus on the immune system are still unclear, however.
To get a better picture of how a serious COVID-19 infection affects the immune system over time, a team led by researchers from Cornell University analyzed blood samples taken from 38 patients recovering from severe COVID-19 and other serious illnesses and compared them to samples taken from 19 healthy people.
The team saw changes to gene expression, or epigenetic changes, in immune cells called hematopoietic stem and progenitor cells (HSPCs). These cells play an important role in the body's first response after infection. The epigenetic changes brought on by COVID caused HSPCs to increase production of monocytes, a type of cell in the immune system.The results provide more evidence of the importance of trying to avoid a serious COVID-19 infection. This means staying up-to-date with the SARS-CoV-2 vaccines. A vaccine targeting newer variants is due out this fall.
The monocytes from people with severe COVID-19 produced more molecules called inflammatory cytokines than those from people with other serious illnesses or those from healthy people. Monocytes produced more inflammatory cytokines for up to a year after SARS-CoV-2 infection.
These changes to HSPCs may explain why people with long COVID have high levels of inflammation throughout their body and why COVID-19 damages organs such as the lungs and kidneys, said the researchers. “HSPCs can pass these epigenetic ‘memories’ on to their daughter cells, changing those cells' inflammatory programs,” Steven Josefowicz, an author on the study, told TheDoctor.
When these modified daughter cells see another disease-causing bacteria or virus, they respond differently from daughter cells that came from unmodified HSPCs, he explained.
The researchers believed an inflammatory cytokine called IL-6 might be the reason for these epigenetic changes. To test this hypothesis, they did experiments in mice with COVID-19-like disease and people with COVID-19.
The researchers characterized these changes at the cellular and molecular level using a method they developed to isolate and enrich the small number of HSPCs that circulate in the blood. This method may make painful and invasive bone marrow biopsies unnecessary in the future, Josefowicz said.
The hope is that this method will be used to study the association between these kinds of epigenetic changes and different disease outcomes in the future. Said Josefowicz, “Since monocytes are more plastic than people first thought, it may be possible to return them to a healthier state after an infection.”
The study is published in Cell.