As people age, their bones often lose density and mass and become brittle and vulnerable to fracture, a condition we call osteoporosis. It is most commonly seen in postmenopausal women but may also develop in men.
There are a variety of medications to help slow or prevent bone loss, but they each have side effects that must be weighed against their benefits. A newly published investigation offers an analysis of nearly 300 studies of the various drugs available to prevent the progression of osteoporosis.
Osteoporosis may also occur in men and women with certain medical conditions such as rheumatoid arthritis or who are on medications such as steroids. Other risk factors include a family history of fractures, race (it is more common among people of European and Asian descent), cigarette smoking, low body weight, and, as mentioned earlier, increasing age.There are steps you can take to decrease the occurrence and impact of this disease.
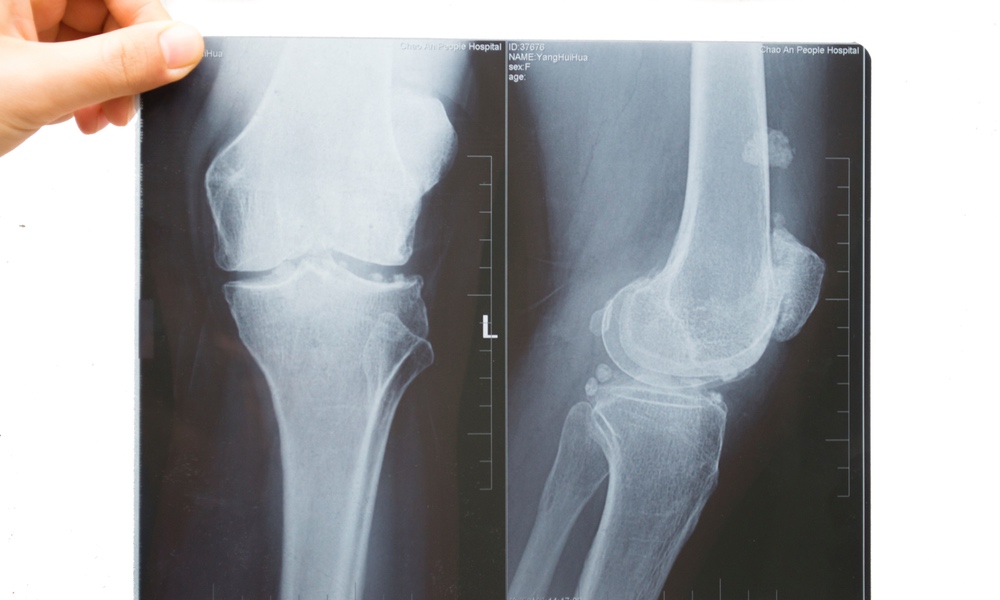
The spine, the ribs, hips, shoulders, and wrists are the most common locations for fractures. When fractures do occur, they often cause the person significant disability and loss of independence. They can also lead to other serious and painful health complications such as spinal cord compression symptoms, deep vein thromboses, and infections.
Osteoporosis has no symptoms in its early stages. Bone loss can be discovered before a fracture occurs by a bone mineral density test. The results of this test are reported as T-scores. These scores are based on a comparison of an older (65+) person's bone density with that of healthy young women. A T-score of -1.0 or higher is normal. A T-score between -1 and -2.49 indicates the early thinning of bones. T-scores of -2.5 or more indicate osteoporosis.
There are steps you can take to decrease the occurrence and impact of this disease. The National Osteoporosis Foundation (NOF.org) recommends getting enough calcium and vitamin D, controlling the amount of protein, sodium and caffeine in your diet, maintaining an active life style, avoiding smoking and excessive alcohol, maintaining a healthy body weight.
Certain medications for other conditions can have a negative effect on bone mass — some antacids and protein pump inhibitors (PPI), some antidepressants, some hormone preparations, chemotherapy drugs, among others. If you have been prescribed drugs that are known to contribute to a loss of bone density, you need to let your healthcare provider know so she can discontinue or alter the dose of these medications. It can be a delicate balancing act, and a doctor's oversight can help patients select the best drugs for their situation.
One major class of drugs that are used to treat osteoporosis is the bisphosphonates. Some examples are: alendronate (Fosamax, Binosto), risedronate (Actonel, Atelvia), ibandronate (Boniva), zoledronic acid (Reclast, Zometa).
A second category are hormone-related medications such as the estrogens used for hormone replacement therapy and raloxifene (Evista) which is similar to estrogen without some of the associated risks. Additionally, teriparatide (Forteo) is similar to parathyroid hormone and acts to stimulate new bone growth and denosumab (Prolia) targets a different step in the bone remodeling process than other medications.Choosing among the options can be challenging as each class of medications is associated with a range side effects from bothersome to potentially disabling.
Raloxifene did not prevent non-vertebral fractures, and there was less evidence to support ibandronate’s effectiveness against non-vertebral fractures relative to the other options. Recent studies have demonstrated that zoledronic acid has moderately strong evidence for prevention of vertebral fractures in men with osteoporosis. Most of the drugs tested were more effective than taking Vitamin D or calcium supplements to prevent fractures.
They found the risk of atypical hip fractures due to medication is much smaller than the risk of osteoporosis-related hip fractures in untreated women, making that risk-benefit data important in making informed treatment choices.
Denosumab also showed a moderate tendency toward causing infection. More seriously, atypical hip fractures at the end of the femur nearest the hip joint, and osteonecrosis of the jaw, a severe bone disease that affects the mandible and maxilla (jaw bones), have been associated with bisphosphonate use.
While the recent study confirmed this connection, it noted that the incidence of either side effect is low and can be reduced if the length of treatment with bisphosphonates is not prolonged. And since it is also true that the risk of atypical hip fractures is much smaller than the risk of osteoporosis-related hip fractures in untreated women, that risk-benefit data are important in making informed treatment choices.
One study showed that when women continued treatment with alendronate for ten years, their risk for non-vertebral fractures was not significantly different, but their risk for clinical recognized vertebral fractures was much lower than for women who stopped treatment after five years.
The researchers conclude that there is good quality evidence to support the use of a variety of drugs for the treatment of osteoporosis for the prevention of vertebral and non-vertebral fractures.Patients who do not yet show serious bone loss will still want to review their risk factors for osteoporosis-related fractures with their healthcare providers.
They note that side effects vary among the drugs. There are too few studies to conclusively compare one medication to another directly, according to the researchers, but they report that the differences between the clinical efficacy of bisphosphonates, denosumab and teriparatide are likely to be modest. The research is published in Annals of Internal Medicine together with an editorial pointing out that the relative risks and benefits among those 75 and older were not part of the current meta-analysis.
Women and men with thinning bones should discuss various options with their medical providers before embarking on a course of therapy. Similarly, those who are experiencing unacceptable side effects may wish to discuss changing to a different type of medication.
Patients who do not yet show serious bone loss will still want to review their risk factors for osteoporosis-related fractures with their healthcare providers so they can identify those risks they may be able to decrease by medication and lifestyle choices.