It can be hard for people who suffer from depression and other mental health problems to find help in a country with only 10 psychiatrists and 15 clinical psychologists. That's the situation in Zimbabwe. The country has found an answer in the problem-solving therapy offered by the Friendship Bench.
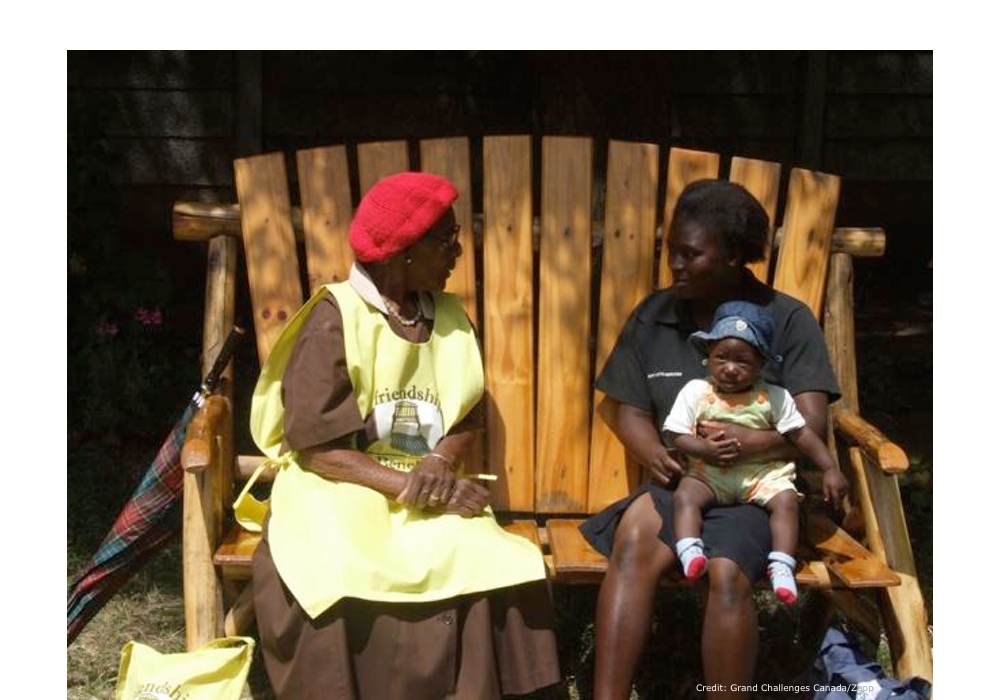
Patients sit on an outdoor wooden bench instead of a psychiatrist's couch. And the therapists are called “Grandmothers.” The mental health workers are trained to listen to and support people living with anxiety, depression and other common mental disorders. They bring the benefits of a simplified form of cognitive behavioral therapy to thousands of people.
Patients who received problem-solving therapy through the Friendship Bench were more than three times less likely to have symptoms of depression after six months, compared to patients who received standard care. They were four times less likely to have anxiety symptoms and five times less likely to have suicidal thoughts than the control group after follow-up. The program may even offer some lessons for the mental health care systems of more developed nations.“In many parts of Africa, if you are poor and mentally ill, your chances of getting adequate treatment are close to zero.”
The manual teaches basic counseling skills such as empathy, patience, the ability to listen well and the ability to ask questions. It also contains information on specific mental health issues such as depression and suicide, as well as standard diagnostic questionnaires (scales).
Treatment principles used on the Friendship Bench are drawn from cognitive behavioral therapy. The patient describes a problem and is encouraged to come up with as many potential solutions as possible. The more ideas, the better the chance that one or two will work.
Patient and therapist thoroughly analyze these solutions, and then one is chosen and they come up with an action plan. The shape of future sessions depends on how well this plan actually works.
The trial looked at 573 patients in 24 clinics. Half of the patients received standard care, while half received the Friendship Bench intervention — six weekly, 45-minute, problem solving sessions, plus six optional group sessions.
Six months later, symptoms were assessed by questionnaire. Fifty percent of patients who received standard care still had symptoms of depression compared to 14 percent who received Friendship Bench. Forty-eight percent of patients who received standard care still had symptoms of anxiety compared to 12 percent who received Friendship Bench, and 12 percent of patients who received standard care continued to have suicidal thoughts compared to 2 percent who received Friendship Bench care.
To date, over 27,500 people have availed themselves of Friendship Bench treatment. In 2017, it will hopefully be available in wider areas of Zimbabwe, including Masvingo province and the refugee centers of the eastern highlands that border Mozambique.
An article on the trial appears in JAMA, the Journal of the American Medical Association.