When you think of it, it makes perfect sense that two doctors in training should write one of the best introductions to the current U.S. healthcare system. Who better to know the ins and outs of inpatients and outpatients, medical research and technology, health insurance, and health policy than two people entering the field?
Nathan Moore and Elisabeth Askin are students in the M.D. program at Washington University School of Medicine. They wrote The Health Care Handbook because they couldn't find a decent introduction to our enormous, convoluted, and incredibly expensive system.
You may think you can avoid the health care system, but ultimately, you can't, so it is a good idea to know the 31 different healthcare professions making up this system, and how the big pharmaceutical companies fit into it. Where else can you can discussions of medical malpractice, the economics that make health care expensive, how hospitals are set up, and the medical device industry? An added bonus is the fact that the book covers the recent Supreme Court decision regarding the Affordable Care Act as well as healthcare policy and reform.
Even-handed and scrupulously researched, The Health Care Handbook is accessible, at times humorous, and, at 240 pages, concise.
A major expansion of health insurance coverage due to the ACA and a rapidly aging population will significantly increase demand for medical services in the coming years, and a number of national organizations have recently sounded alarms that the supply of physicians won’t be able to keep pace. One of these organizations, the Association of American Medi- cal Colleges, forecasts a shortfall of 130,000 physicians by the year 2025. In addition, the unequal distribution of physicians throughout the country means that some areas are already experiencing a shortage; the federal government already designates more than 20% of the U.S. population as living in a “health professional shortage area.” A national consensus is growing that the supply of physicians needs to be expanded, but to do so will require changes to an already controversial system.
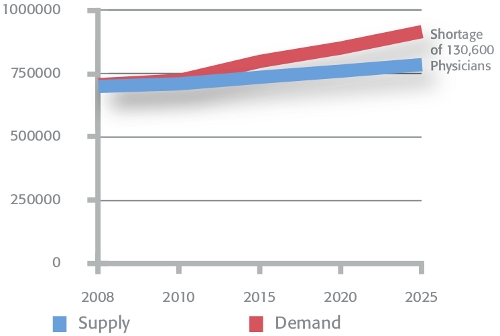
Association of American Medical Colleges, “Physician Shortages to Worsen Without Increases in Residency Training,” September 2010. Used by permission.
In 2010, there were 79,020 medical students in the U.S., of whom 18,665 were newly enrolled. That same year, there were 113,142 medical resi- dents in the U.S. (There are more residents than students because many residencies are longer than the four years of medical school and also because many residencies are filled by international medical graduates.) Many more people would like to become physicians, but the bottleneck (and barrier) to actually becoming one is the limited number of medical school and residency slots, which in turn limits physician supply and con- tributes to the shortage.
The number of residents is limited by two main entities: first, by the Department of Health & Human Services, which, largely through Medicare, funds most residency programs; second, by the Accreditation Council for Graduate Medical Education (ACGME), which approves any new resi dencies in each specialty through Residency Review Committees. There are arguments both for and against limiting the number of medical students and residents (which is, ultimately, a limit on physicians). Here’s a point-counterpoint summary of the arguments.
| Point: Limiting Physician Number is Good | Counterpoint: Limiting Physician Number is Bad |
|---|---|
|
|
The percentage of U.S. physicians choosing to work in primary care has been on the decline for some time, and today less than 40% of practic- ing physicians are in primary care. The reasons for this trend are many: higher pay for specialists than for primary care physicians (PCPs), the low status of primary care in most academic medical centers, and unpleasant workloads (too much paperwork, too many patients per day). Compound- ing the problem, hundreds of primary care residency slots have been cut or converted to specialty training positions, ensuring that the number of new PCPs will fall.
and Other Doctors as a Share of Total Doctors

Organisation for Economic Co-operation and Development
“Health Data 2011,” June 2011.
Note: Specialists include pediatricians, ob/gyn, psychiatrists, medical specialists and
surgical specialists. Other doctors include interns/residents if not reported in the field in
which they are training, and doctors not elsewhere classified.
Cost: In 2005, a systematic review of research about primary care usage and health outcomes found that “areas with higher ratios of primary care physicians to population had much lower total health care costs than did other areas, possibly partly because of better preventive care and lower hospitalization rates. [...]In contrast, the supply of specialists was associ- ated with more spending and poorer care.”
Access: Primary care is the easiest way for most people to access health ser- vices, both for ongoing wellness or disease management and for appropriate referrals to specialists. In rural areas, if there’s a shortage of primary care physicians, then there’s almost certainly a shortage of specialists as well.
Quality: Use of primary care leads to better health outcomes. The same systematic review as above found that primary care was associated with better outcomes in all-cause mortality, heart disease mortality, stroke mortality, infant mortality, low birth weight, life expectancy, and self-rated health. Primary care creates this benefit through six mechanisms:
- Greater access to needed services
- Better quality of care
- A greater focus on prevention
- Early management of health problems
- The cumulative effect of the main primary care delivery characteristics
- The role of primary care in reducing unnecessary and potentially harmful specialist care
From this list, one can conclude that a shortage of primary care providers may lead to poor quality, high costs, and restricted access. Health care reform may only exacerbate this problem—over the next decade, millions of newly insured Americans will be looking for primary care providers. They may be in for a rude surprise when they find that many primary care pro- viders won’t take new patients with Medicare and Medicaid (see Under- payment on page 118), and of those that do, the wait for an appointment may be one month or more.
- Make medical education free.
- Encourage and incentivize medical students to enter primary care.
- Tweak current payment systems (like Relative Value Units, page 93) to increase reimbursement for primary care services.
- Use alternate payment systems (like capitation, page 92) that reward health promotion and coordination of care rather than costly procedures.
- Reduce the hassles of primary care practice (e.g., less paperwork, longer patient visits, etc.).
- Increase the number of residency positions in primary care training programs.
- Shift more of the primary care workload to nurse practitioners (page 57) and physician assistants (page 66).
- Expand the Patient-Centered Medical Home and other delivery structures that put the PCP in charge of coordinating patient care across medical specialties.
- Establish more three-year medical schools—cheaper and faster— aimed at producing family physicians.




