Dr. Wolf is Assistant Professor of Medicine, Department of Medicine, Downstate Medical Center, Brooklyn, New York.
As more and more people in many countries are maintained by current kidney replacement therapies, the medical and economic burdens caused by chronic kidney failure continue to grow. Although approximately 700,000 patients in the United States alone, as of December 31, 2003, were receiving treatment for end stage renal disease (ESRD)] (see Figure 1), their annual survival has not really improved over the past decade because other associated diseases such as heart failure, cancer, infection are now much higher as shown in Figure 2.
Figure 1.
Total Number of Patients with ESRD in the United States on December, 2003.
USRDS Annual Data Report 2005.
Figure 2.
Death Rate By Cause in the United States.
During the next decade, the number of new cases of ESRD in the U.S. is projected to double, driving costs way beyond the current $18 billion annually.
In developing nations, the actual number of patients receiving renal replacement therapy is unknown. What is clear, however, is that given the high costs of both maintenance hemodialysis and kidney transplant, most of the world is unable to afford therapy for failing kidneys.
Figure 3.
Cost per Patient Year by Modality of Renal Replacement Therapy.
Patients = 452,957
Deaths = 82,588
Medicare $ Per Patient
| Hemodialysis | Peritoneal Dialysis | Kidney Transplant |
|---|---|---|
| $63,000 | $43,000 | $95,587 |
Medicare Total $18.3 billion
Source: USRDS 2005.
Indeed, as charted by the World Health Organization and the Central Intelligence Agency Data Base, life expectancy follows income (see Figure 4).
Figure 4.
Life Expectancy Is Higher in Nations with Higher Gross National Income, from World Bank and CIA.
GNI = gross national income per person, World Bank April, 2003.
Life Expectancy, World Factbook 2003, Central Intelligence Agency, May 31, 2003.
The number of patients with ESRD who gain treatment is closely linked to annual per person income. The citizens in the wealthiest countries presently die from heart disease and not from kidney failure. Yet despite improved dialysis and support care, patients need new kidneys of some sort because kidney failure remains deadly with more than 50% of patients dying from the disease. Since there are now more patients on dialysis, waiting time for a deceased donor kidney transplant has lengthened significantly (to a decade in the New York region). As a consequence, physicians have increasingly relied on transplantable kidneys harvested from donors previously excluded because of advanced age or other disorders and from living unrelated donors. But, nevertheless, these remedies fall short of meeting the need for donor kidneys.
Given the expanding demand for kidney replacement therapy, medical scientists are attempting to devise innovative, low cost regimens that go beyond dialysis and which may truly replace renal function. Whatever the solutions, researchers realize that they be must be affordable within developing nations.
Normal Kidney Function
In health, normal kidney function maintains a careful balance (homeostasis) of body composition in response to changing intake of food and water. At the same time, the kidney provides vital hormone and disease-fighting functions, as illustrated in Figure 5.
Figure 5.
Metabolic Kidney Functions.
| Excretory | Secretory |
|---|---|
| Minerals, Water Nitrogenous wastes Toxins, Medications |
Enzymes, Vitamin D Erythropoietin Prostaglandins |
Figure 6.
Illustration of Native Kidney.
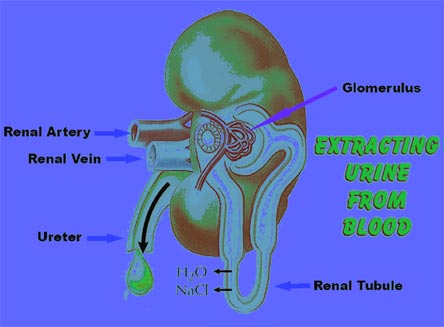
Each nephron adds or removes the body chemicals and waste products from the blood, reclaiming (resorbing) what is needed, while discarding (excreting) what is no longer necessary for health, as well as managing water elimination. Hormones secreted by the kidney include renin, which has a role in blood pressure control, erythropoietin, which helps make new red blood cells, prostaglandins and 1,25-dihydroxy vitamin D. Additionally, the kidney is a source of cytokines (proteins which help fight infections) including nitric oxide and endothelin, and contributes to key metabolic processes such as the synthesis of new sugar.
Currently Available Renal Replacement Therapy
In wealthy nations, kidney patients have three available options of replacement therapy, with a fourth option — no therapy — that implies near term death. A functioning kidney transplant is the best option but, as noted above, is unavailable for the majority of ESRD patients. Dialysis therapies extract clear water and small molecules such as sodium and urea but rely on outside support care to provide the required hormones and metabolites. Thus a typical ESRD patient receives regular injections of red cell building hormone erythropoietin at the time of hemodialysis and ingests synthetic vitamin D. Dialysis-treated ESRD patients, however, lack the kidney's natural ability to help with infections.
Stem Cells and the Kidney
Most viable therapies for kidney failure are based on the use of stem cells.9 Stem cells are basic building block cells that can self-renew and "grow" into specialized cells. In terms of kidney therapy, the ultimate goal of stem cell researchers would be the production of a new kidney. This is a difficult challenge because the kidney is made from several very different cell types, each with its own special function.
Figure 7.
Proximal Tubular Cells in Culture.

Bioartificial Kidney
The renal tubule assist device (RAD), developed by H. David Humes at the University of Michigan, consists of a man-made blood filter connected to a cartridge containing approximately one billion human kidney cells. These proximal tubular cells can perform some of the kidney's important blood cleaning functions.
Figure 8.
RAD Device.
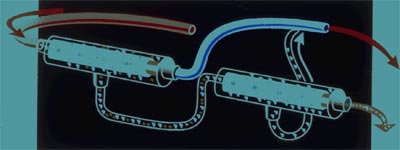
A hemodialysisfilter connected in series with proximal tubular cells. Arrow points to the direction of blood flow.
Courtesy of H. David Humes.
Courtesy of H. David Humes.
Early experiments with dogs who had kidney failure demonstrated the possible effectiveness of RAD and paved the way for the first use of RAD in 10 kidney patients in an intensive care unit. Recently, a phase II clinical trial in which the RAD device was employed in 58 critically ill patients on dialysis was completed. The results were impressive but need to be confirmed in a larger study.
Nanomedicine
The marriage of biology to advanced modern technology yielded another development that may alter the direction of clinical nephrology — the human nephron filter (HNF). This experimental artificial membrane is based on nanotechnology, which develops anatomically precise, very tiny (one-billionth of a meter), functional machine systems. A conceptual drawing is provided in Figure 9.
Figure 9.
Wearable Human Nephron Filter.
In the center is the device with the artificial membranes. A high capacity battery would be worn on a belt and vascular access would be obtained as in conventional dialysis.
From Hemodial Int. 2005: 9(3);210-7.
From Hemodial Int. 2005: 9(3);210-7.
Bioencapsulation
Another form of biotechnology that holds promise in the treatment of kidney failure is the use of so-called bioencapsulated living cells. In one proposed technique, soon to enter human clinical trial, selected bacteria convert nitrogen waste products into non-toxic compounds that may be recycled within the living subject. This is a novel approach to an old idea: using the gut for dialysis, as shown in Figure 9.
Figure 10.
Using Bowel for Dialysis.

Paul Schloerb. 1958.
Given that we still administer activated charcoal by mouth to treat some cases of poisoning, it is not surprising that agents administered by mouth might have application in treating kidney failure. For example, loss of nitrogen wastes through diarrhea-inducing therapy has also been shown to be effective in kidney failure.
The idea to administer encapsulated bacterial enzymes to break down toxic substances was introduced in Finland in 1978. A series of probiotics, foods that contain 'beneficial' bacteria, for example Lactobacillus, found in milk, in combination with oral charcoal and locust bean gum, have been prepared and tested in volunteers as the first oral renal replacement therapy in pill form.
Figure 11.
Renal Replacement Therapy in a Pill.
Summary: Future Options
Kidney failure is treatable even though anatomical damage to host kidneys persists. Currently, available treatment strategies — maintenance hemodialysis or peritoneal dialysis — are prohibitively expensive, and not enough donor organs are available for kidney transplantation. Although the bionic kidney holds great promise, it, too, will be prohibitively expensive and will require very highly trained personnel. It is therefore necessary to develop new approaches to replace renal function that the world can afford.




